Overview
The skeleton of the human being is a unique structure that has adapted to the needs of bipedal locomotion and erect posture. The structural peculiarities of the human skeleton give human beings their characteristic appearance and facial geometry.
The bony skeleton provides the shape and framework on which the human body is designed and functions. It houses and protects vital organs; it contains bone marrow, which is the functional unit of the hematopoietic system; and it provides attachments and anchorage to muscles and ligaments and joint capsules. Bones often act as levers, which, in conjunction with muscular contraction, initiate and sustain movement.
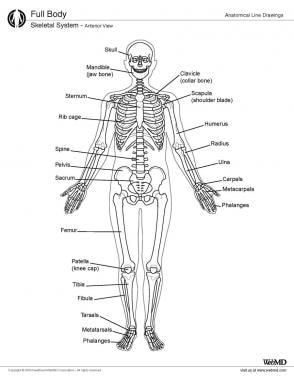
This article provides an overview of the basic anatomy of the human skeleton, bones, and joints (see the image below).
Gross Anatomy
The bony skeleton is divided into 2 parts: the axial skeleton and the appendicular skeleton. The axial skeleton is the central core unit, consisting of the skull, vertebrae, ribs, and sternum. The appendicular skeleton comprises the bones of the extremities. The human skeleton consists of 213 bones, of which 126 are part of the appendicular skeleton, 74 are part of the axial skeleton, and 6 are part of the auditory ossicles. [1]
Bone is a solid organ that appears pinkish white externally and deep red internally when in a fresh state. [2] Essentially, bone is of 2 types, compact (or cortical) bone and cancellous (or woven) bone. The relative quantities of compact and cancellous bone vary in different locations, depending on the relative requirements for strength and flexibility, respectively, at a given site.
As the name suggests, compact (cortical) bone is well-packed and densely organized bone. It appears ivorylike and is very strong. This type of bone is mainly found in the diaphyses of long bones. Cancellous (woven) bone, on the other hand, has loosely woven lattices with relatively less dense organization of the bone tissue. Cancellous bone is found in the epiphyses and metaphyses of long bones, among other locations.
Anatomically and structurally, the different types of bone are traditionally grouped as follows:
-
Long bones - Clavicle, humerus, radius, ulna, metacarpals, femur, tibia and fibula, metatarsals, and phalanges; the metacarpals, metatarsals, and phalanges are sometimes referred to as short long bones
-
Flat bones - Skull, mandible, scapula, sternum, and ribs
-
Short bones - Carpal and tarsal bones, patella, and sesamoids Irregular bones - Vertebrae, sacrum, coccyx, and hyoid bone
The long bone itself has different parts, as follows:
-
Diaphysis - This is the central and cortical shaft of a long bone; the narrowest part of the diaphysis is often referred to as the isthmus of the long bone.
-
Metaphysis - The diaphysis flares on either side to form the metaphysis, which is essentially cancellous bone
-
Epiphysis - This lies on either end of the long bone; in the adult, it is the remnant of the growing end of the long bone, whereas in a child, the ends of the long bone possess the growth plate and the epiphyses
-
Medullary cavity - This is the cavity within the long bone; it contains bone marrow and its constituents
Bone is covered by a membrane called the periosteum. The inner medullary cavity is lined with a membrane called the endosteum.
The periosteum, as described by Gray, has multiple small vessels tethering it to bone; these vessels provide a major part of its blood supply. The periosteum is attached to bone by fine fibers called Sharpey fibers. It constitutes a fibrous connective tissue sheath that surrounds the outer cortical surface of bone, except at joints, where bone is lined by articular cartilage. The periosteum contains blood vessels, nerve fibers, osteoblasts, and osteoclasts. It is thicker in children than in mature adults.
The periosteum is a vital structure in bone function, serving to nourish and protect the underlying cortical bone. This function is especially evident with subcutaneous bones like the tibia: when such bones are exposed and injured, their very survival may depend on the presence or absence of periosteum. Periosteum is essential for appositional growth and remodeling of bone. Because bone resorption typically exceeds bone formation as a person grows older, the medullary canal appears to widen with increasing age.
Images depicting the anatomy of the adult skeleton can be seen below.
 Anterior view of lumbar spine, showing lumbar vertebrae, curvature of lumbar spine, sacroiliac joints, and iliac wings. Pelvic inlet is partially visualized.
Anterior view of lumbar spine, showing lumbar vertebrae, curvature of lumbar spine, sacroiliac joints, and iliac wings. Pelvic inlet is partially visualized.
 Cervical spine, as seen from side, showing anatomy of cervical vertebrae and lordotic alignment of cervical spine.
Cervical spine, as seen from side, showing anatomy of cervical vertebrae and lordotic alignment of cervical spine.
Joints
The ends of bones articulate to form mobile (or, sometimes, nonmobile) units termed joints (see the images below). These are essentially the connections between the bony elements of the skeleton. In terms of the type of tissue that bridges them, joints may be described as synovial or fibrous, cartilaginous, or bony.
 Hip, as seen from lateral side, showing trochanter and acetabular lip. Posteriorly, ischial tuberosity is well seen.
Hip, as seen from lateral side, showing trochanter and acetabular lip. Posteriorly, ischial tuberosity is well seen.
Synchondroses are cartilaginous joints (eg, the sternocostal joint). Synovial joints are lined by a specialized membrane called the synovial membrane and the articulating ends of the bones are lined by specialized cartilage termed hyaline cartilage. This makes the joint specially suited for mobility. Lubricating synovial fluid is secreted by the synovial membrane (columnar epithelium). This fluid also nourishes the articular cartilage, which has sparse blood supply. Repetitive joint movements in synovial joints allow the synovial fluid to replenish itself and maintain cartilage function. Examples of synovial joints include the knee, hip, elbow, and atlanto-axial joint.
The articular cartilage is itself not innervated.
The ends of long bones that articulate with each other are often flared to form bulbous projections called condyles. These are lined by articular or hyaline cartilage.
Vasculature
Bone derives its blood supply from nutrient arteries, which enter the medullary canal at fixed points in the cortex. A number of apertures may be found on the surface of the bone, many of them representing points where veins exit from the surface of the bone. These apertures are found more often at the metaphyseal ends of the long bones. In the flat bones of the skull, these venous channels are numerous and run within tortuous channels in the diploic tissue.
Microscopic Anatomy
Bone is composed of an organic and an inorganic phase. The organic phase is formed by cells and the collagen-forming part of the matrix. The inorganic phase contains hydroxyapatite, calcium salts, and other minerals. The bone essentially then works as a reservoir of calcium, which is important for most metabolic functions in the human body.
Structure of bone
Microscopically, cortical bone is made up of osteons. The osteons are made up of haversian systems, which are concentric lamellae of bone surrounding a central haversian canal. These lamellae are often called by different names, depending on their location; they may be interstitial lamellae, primary or fundamental lamellae, or circumferential lamellae. Haversian canals run longitudinally down the bone. They connect to the subperiosteal space via Volkmann canals and to each other via canaliculi.
Cancellous bone, on the other hand, is composed of bony trabeculae that run along the lines of stress. These are best visualized in cross-sections of the vertebral body and femoral neck, where the trabecular pattern demonstrates the line of weight transmission.
Structure of bone marrow
In the diaphyses of long bones, the bone marrow is yellow and contains predominantly fat, along with some marrow cells and some connective tissue. In the ends of long bones and in flat bones, the marrow is red and is made up of 75% water and 25% solid matter, which includes a very small amount of fat. [2] The cellular content of the red marrow consists primarily of rounded nucleated cells—the true marrow cells, or, as Gray calls them, the marrow cells of Kolliker (or myelocytes). These are the true precursor cells.
Other cells in the marrow include erythrocytes and giant cells. The giant cells excavate small cavities in the bone called Howship's lacunae. They are concerned with bone resorption and are called osteoclasts. Cells concerned with deposition of bone are called osteoblasts. They function in concert not only in the process of bone formation but also in the process of continuous bone remodeling throughout life.
Natural Variants
Adaptation to the bipedal posture has brought about some changes in the human skeleton as compared with quadruped skeletons.
For example, the curvatures of the spinal column are adaptations that serve to facilitate erect posture and maintain the center of gravity. The cervical spine is lordotic (concave anteriorly), and the thoracic spine has a reverse curvature and is kyphotic (convex anteriorly). The lumbar area once again becomes lordotic, and the curvature reverses sharply yet again in the sacrum. These curves are not to be found in the fetal skeleton, where the spine has a single convex posterior curve.
The upper limbs are designed to enable sophisticated movement of the hand in space so as to serve the unique prehensile and fine activities that can be performed with the upper limb. The multiaxial shoulder joint and the uniaxial elbow joint allow the forearm and hand to be positioned for optimal function.
The surfaces of long bones and flat bones have ridges and surfaces that are formed by the attachments of muscles and ligaments. Bulbous offshoots (eg, trochanters and tuberosities) are also formed at sites of muscle attachments and fascial and ligamentous attachments. These offshoots are specific to each bone, depending on the bone's relations with its surrounding soft tissues.
Clinical Significance
A break in the continuity of a living bone is a fracture. These fractures can occur in practically every bone. Fractures usually occur as a result of significant trauma. The direction and intensity of force determines the degree of damage to bone. Bone injuries invariably damage the soft tissue in the vicinity to variable extents. This may include damage to muscles, nerves, blood vessels, and the skin envelope. Significant damage to the soft tissue envelope renders the fracture site susceptible to infections and further morbidity; these are called open fractures. Loss of periosteum also influences the ability of bone to heal in these cases.
Sometimes, fractures occur through areas of bone weakened by pathological processes, and these are called pathological fractures. Pathological fractures occur through areas of bone weakened by systemic or local pathologies. Systemic pathologies that can weaken bone vary from osteoporosis (a decrease in bone mass per unit volume), osteomalacia (a decrease in the mineralization of the osteoid, occurring because of nutritional deficiencies, an adult variant of rickets), and hyperparathyroidism, among others. Local pathology causing weakening of bone varies from infections to benign neoplasms and malignant tumors. These fractures are treated differently from the usual traumatic fracture, the management being dictated by the pathology and its prognosis.
The normal anatomy of bone is exploited in the management of various injuries of bone. Intramedullary fixation is the standard of treatment of long bone diaphyseal injuries in the lower limb. The isthmus, which is the narrowest part of the long bone, is the main obstacle to passage of an intramedullary device and must be widened by a process called sequential reaming, which enlarges it to accommodate the largest possible fixation device. Intramedullary fixation is performed without opening the fracture site and allows speedy rehabilitation of long bone injuries like femoral and tibial fractures.
The introduction of an implant into the medullary cavity can increase the pressure within the medullary cavity high enough to force fat globules into the blood circulation. This is called fat embolism. It can occur during procedures of intramedullary reaming, during nailing procedures, or during the implantation of a prosthetic device in joint replacement.
Metaphyseal and metaphyseodiaphyseal fractures are treated with plates applied to the surface of bone and fixed with screws. Current developments have made available multiple anatomically precontoured plates to fix juxtaarticular injuries. Some of these are the proximal tibial anatomical plate, anatomical plates for fixation of the distal humerus, proximal humeral anatomical locking plates (PHILOS), mini-fragment plates for small long bones, and others, providing extensive options for the management of specific injuries.
Some diaphyseal injuries like those in the humerus and the radius and ulna are best managed by fixation with plates and screws as these allow speedy restoration of function with minimum postoperative immobilization.
Significance of Joint Injuries
Articular injuries are different from diaphyseal injuries. Articular injuries extend into the joint space and disrupt the articular cartilage.
In addition, there may be articular injuries to the ligaments and cartilage that further compromise the joint.
Articular injuries require speedy and accurate reconstruction of articular surfaces with restoration of normal alignment. Nonanatomical healing of the articular surface causes irregularities of the articulating cartilage and subsequent early onset of osteoarthritis.
Joint injuries are also associated with a potential for stiffness and disability consequent to the loss of range of motion. It is therefore imperative that articular and juxtaarticular injuries be treated with modalities that allow early restoration of joint motion and early rehabilitation. This precludes most nonsurgical methods of treatment.
Early range of motion after accurate anatomical alignment and stable fixation of intraarticular fractures allows the cartilage to heal without defects and prevents the formation of intraarticular and extraarticular adhesions, thus minimizing disabilities.
Ligament injuries to weight-bearing joints have a similar impact on the articular cartilage. Instability causes repeated and unnatural wear and tear leading to early onset of osteoarthritis. Such a picture can be seen with long-standing anterior cruciate ligament tears in the knee or following meniscectomy.
-
View of human skeleton from behind, showing rib cage and spine.
-
Anterior view of lumbar spine, showing lumbar vertebrae, curvature of lumbar spine, sacroiliac joints, and iliac wings. Pelvic inlet is partially visualized.
-
Lumbar spine, as seen from side.
-
Lumbar spine, as seen from behind.
-
Cervical spine, as seen from behind, showing arch of atlas and cervical vertebrae.
-
Cervical spine, as seen from side, showing anatomy of cervical vertebrae and lordotic alignment of cervical spine.
-
Craniocervical articulations.
-
Hip, as seen from lateral side, showing trochanter and acetabular lip. Posteriorly, ischial tuberosity is well seen.
-
Hip joint: ball-and-socket articulation.
-
Knees, as seen from front, showing normal valgus alignment of tibiofemoral articulation.
-
Knee, as seen from side.
-
Shoulder: highly mobile ball-and-socket joint with multiaxial movements.
-
Skeletal system, anterior view.
-
A pathological fracture through a benign cyst in the proximal femur.
-
A comminuted intraarticular fracture of the distal femur and proximal tibia.